Struggling with blurry vision due to corneal damage?
Preparing for Corneal Surgery? Cornea surgery can restore clarity from infections to keratoconus, several conditions may require treatment.
If you are planning for corneal surgery, it is important to be well-prepared to ensure a smooth experience and the best results. At Delhi Eye Centre, Dr. Ikeda Lal and the expert team will guide you every step of the way.
How to prepare for corneal surgery?
· Follow your doctor’s instructions
· Please bring an attendant along, if possible, because your vision might be blurry after the procedure, have a family member or friend for drive your home.
· You should not use any make up on the day of surgery. Take a bath on the day of the procedure as you may have to avoid head bath for a few days after the surgery. You need to keep your face clean and avoid any lotions or perfumes.
· Prepare your questions: If you have any concerns, make a list of questions to discuss with eye doctor.
But the most important thing you need to know?
- What is corneal surgery?
- What the common cause?
- Which surgery is right for you?
Let’s explore the causes, types, and best solutions so you can see the world clearly again! Here’s What You Need to Know!
The Role of the Cornea & Its Value
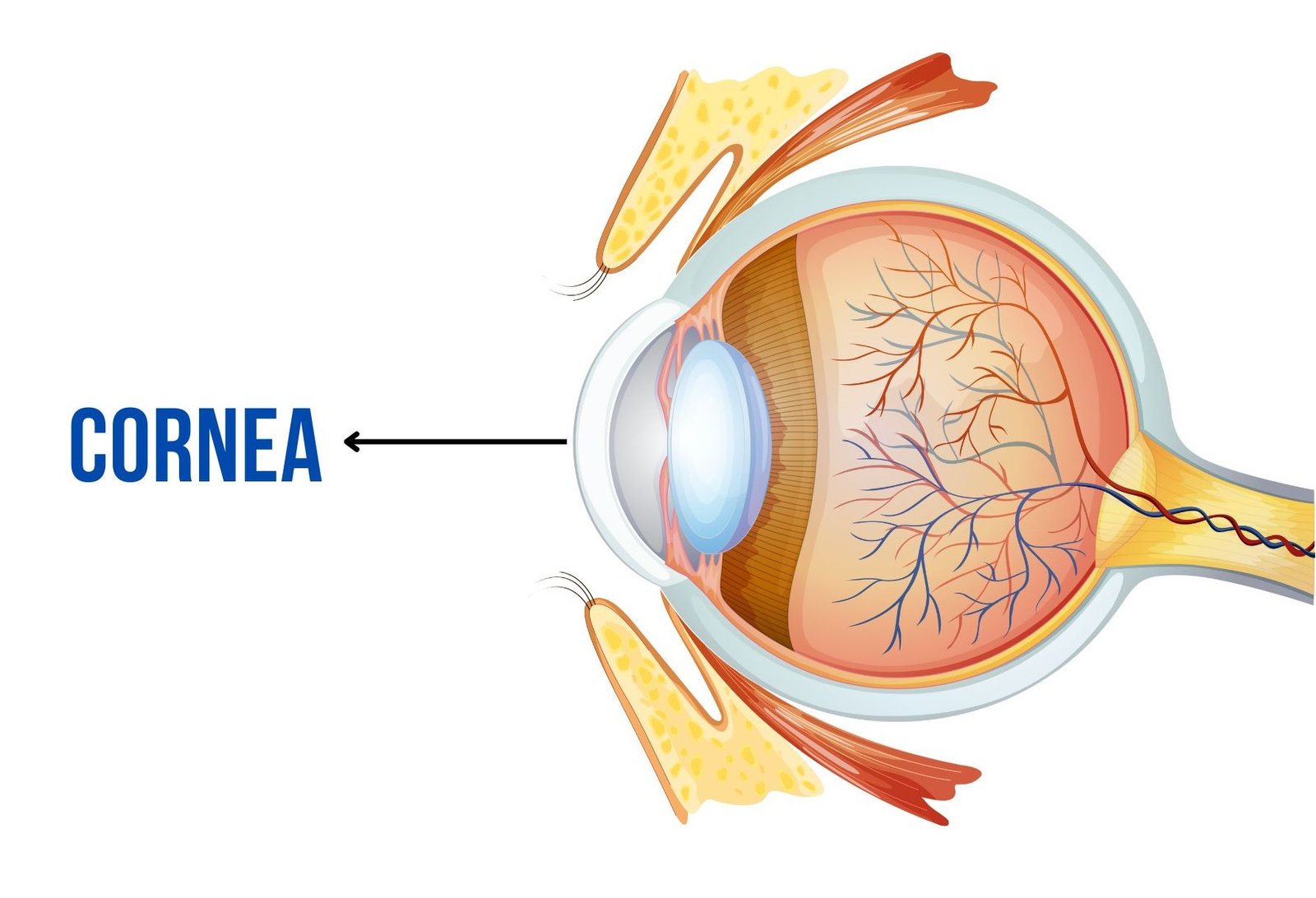
The cornea is the clear front part of the eye, covering the pupil and iris. It provides two-thirds of the eye’s focusing power but remains fixed, while the lens fine-tunes focus. Made up of five to six layers, it stays transparent without blood vessels, getting oxygen from the air through the tear film.
Damage to the cornea from keratoconus, infections, or injuries can blur vision. Corneal surgery, including transplants and cross-linking, can restore clarity and protect your sight!
At Delhi Eye Centre, some of the best cornea specialists in Delhi provide expert care for a wide range of corneal conditions, including dry eye, keratoconus, corneal dystrophies, and allergic or immune-related disorders.
Types of Corneal Transplant Procedures
Different types of corneal transplants are available depending on the severity and location of the corneal damage:
- Penetrating Keratoplasty (PK) : Penetrating Keratoplasty (PK) is a full-thickness corneal transplant where the entire central portion of the damaged cornea is replaced with a healthy donor cornea. This procedure is recommended for patients with severe corneal damage scarring, severe corneal infections. We usually suture the donor corneal tissue in place with the help of 16 sutures, these are gradually removed starting at 3 months. It is very important to use eye drops regularly after PK to avoid graft rejection.
- Deep Anterior Lamellar Keratoplasty (DALK) : Deep Anterior Lamellar Keratoplasty (DALK) is a partial-thickness corneal transplant that replaces the front layers of the cornea while preserving the patient’s own Descemet’s membrane and endothelium. DALK is ideal for patients with keratoconus, corneal scars, or stromal dystrophies, limited to anterior two-thirds of the cornea. Since the patient’s endothelium remains intact, the risk of transplant rejection is significantly reduced compared to full-thickness PK. The post-operative medicines required are also less than PK.
- Superficial Anterior Lamellar Keratoplasty (SALK) : Superficial Anterior Lamellar Keratoplasty (SALK) is a procedure that replaces only the most superficial layers of the cornea, leaving deeper structures intact. It is mainly used for treating anterior corneal scars and surface disorders. This technique minimizes complications, reduces recovery time, and provides faster healing compared to deeper transplants. Patients with minor corneal surface irregularities often benefit the most from this procedure. A femtosecond laser is used to perform SALK, reducing the number of sutures and therefore the post-operative glass prescription.
- Descemet’s Stripping Endothelial Keratoplasty (DSEK) : Descemet’s Stripping Endothelial Keratoplasty (DSEK) is a selective corneal transplant that replaces only the diseased endothelial layer and Descemet’s membrane while preserving the majority of the patient’s cornea. It is commonly used for endothelial dysfunction conditions such as Fuchs’ dystrophy, pseudophakic bullous keratopathy(PBK). DSEK provides quicker recovery, fewer sutures, and better visual outcomes compared to full-thickness transplants. The procedure has gained popularity due to its lower rejection rates and improved post-operative stability.
- Descemet’s Membrane Endothelial Keratoplasty (DMEK) : Descemet’s Membrane Endothelial Keratoplasty (DMEK) is the most advanced form of endothelial keratoplasty, involving the transplantation of only the Descemet’s membrane and endothelial cells. Since this procedure uses ultra-thin donor tissue, it offers superior visual results and a lower risk of rejection compared to DSEK. However, only a handful of patients are suitable for this procedure. The main indication includes patients with fuchs endothelial dystrophy.
Who Can Benefit from a Corneal Transplant?
A corneal transplant is often recommended for patients with severe corneal damage, scarring, or diseases such as keratoconus, corneal dystrophies, severe corneal infections, Fuchs endothelial dystrophy, pseudophakic bullous keratopathy and corneal perforations. Corneal transplants are among the most successful tissue transplants due to the avascular nature of the cornea.
Why is a Corneal Transplant Needed?
A corneal transplant is necessary when the cornea becomes severely damaged or diseased, leading to impaired vision, discomfort, or pain. Common reasons for corneal transplantation include:
- Keratoconus : A progressive condition that causes the cornea to become cone-shaped and thin, distorting vision.
- Corneal scarring : scarring in the cornea can occur due to infections, injuries, dystrophies that lead to loss of transparency in the cornea.
- Fuchs’ endothelial dystrophy : A hereditary condition that affects the corneal endothelium, causing swelling and vision impairment. Although, it is a hereditary condition, it usually presents around 50 years of age.
- Corneal Decompensation : Swelling of the cornea which can require an endothelial transplant. This can be caused because of cataract surgery or viral keratitis
- Severe corneal ulcers : a corneal infection or ulcer unresponsive to antibiotics may require a therapeutic keratoplasty to control the infection. A keratoplasty may also be required if there is large perforation due to infection, so that the eye can be saved.
Corneal transplants are performed when other treatments, such as medication or specialized contact lenses, fail to improve vision.
Recovery and Post-Operative Care
Recovery time for a corneal transplant varies depending on the type of procedure performed. Full-thickness transplants like PK take longer to heal, often requiring several months for vision to stabilize. Lamellar techniques such as DALK, DSEK, and DMEK offer quicker recovery times, often within weeks or a few months.
Post-operative care is essential for a successful outcome. Patients are prescribed medicated eye drops to prevent infection and rejection. Regular follow-up appointments with a cornea specialist help monitor healing and detect any complications early.
Corneal Surgery Cost at Delhi Eye Centre
Average Cost is ₹70,000 To ₹75,000 per eye
- PK: 65,000 Per Eye
- DALK : 75,000 Per Eye
- FEMTO DALK: 1,20,000 Per Eye
- SALK: 1 Lakh Per Eye
- DSAEK: 75,000 Per Eye
- DMEK: 80,000 Per Eye
- PK+ECCE+IOL: 1 Lakh Per Eye
The final cost may vary based on your specific condition and will be confirmed after a detailed examination of your cornea by the specialist.
Recovery and Post-Operative Care
While corneal transplants have high success rates, rejections can occur. Common warning signs can be membered with a mnemonic RSVP which stands for
- R- Redness
- S- Sensitivity to light (Extreme)
- V- Vision loss / Blurriness
- P- Pain
If you experience any of these symptoms, it is crucial to seek immediate medical attention from a top cornea specialist in Delhi. Early intervention can help prevent transplant failure and preserve vision.
Meet Your Cornea Surgeon: Dr. Ikeda Lal
 Dr. Ikeda Lal, MS, MBBS, FICO, FLVPEI
Dr. Ikeda Lal, MS, MBBS, FICO, FLVPEI
Director, Delhi Eye Centre | Senior Consultant, Sir Ganga Ram Hospital, New Delhi
Specialist in Cornea, Cataract, and Refractive Surgery
- Ikeda Lal is a ophthalmologist with expertise in corneal transplants, cataract surgery, refractive procedures (LASIK, ICL), ocular surface disorders, and lamellar corneal surgeries. She completed her advanced fellowship in cornea and anterior segment at the prestigious L.V. Prasad Eye Institute.
- She currently serves as the Director of Delhi Eye Centre and Senior Consultant at Sir Ganga Ram Hospital, New Delhi. She is also a Senior Instructor at the Annual American Academy of Ophthalmology (AAO) conference for the past five years.
At Delhi Eye Centre, our expert surgeons use cutting-edge techniques and advanced technology to provide the best possible outcomes for corneal surgeries. Whether you need treatment for a corneal disorder or a transplant, we are committed to delivering world-class eye care.
